Fetal surveillance consists of a
number of tests used to assess the health of babies in the womb, and has been a part of obstetric care since the 1970s.
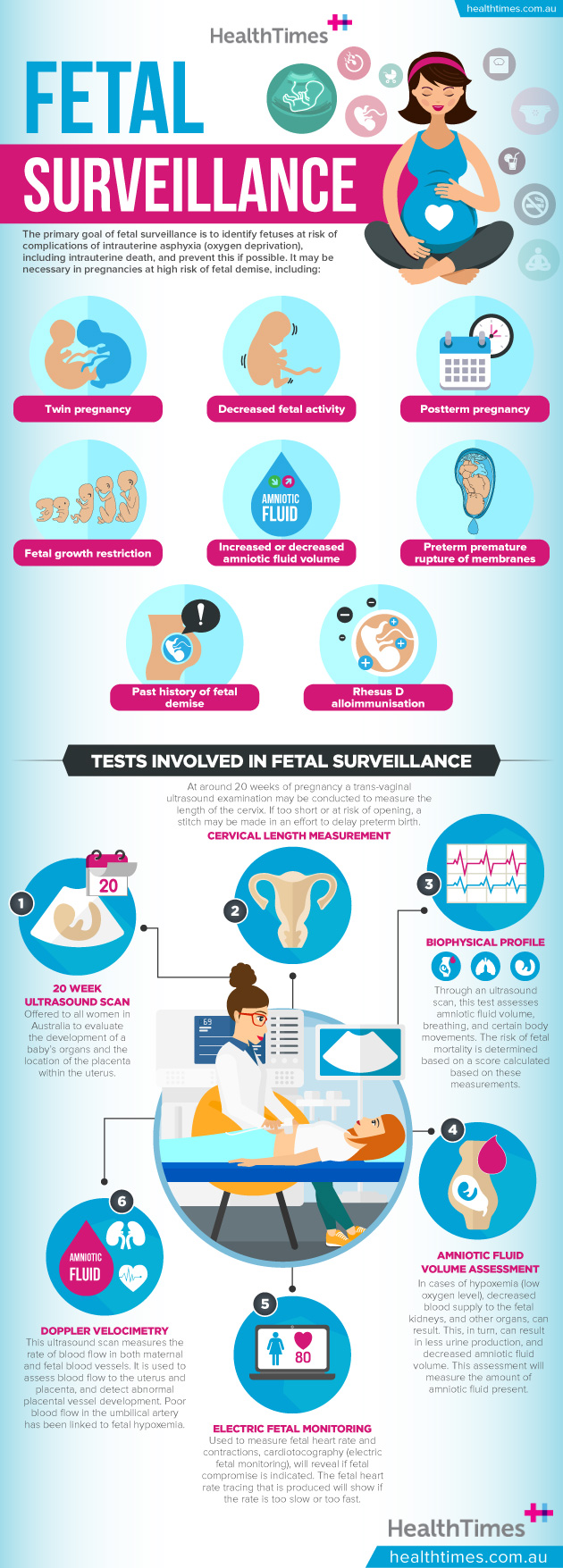
The primary goal is to identify fetuses at risk of complications of intrauterine asphyxia (
oxygen deprivation), including intrauterine death, and prevent this if possible. This may be detectable as fetuses generally respond to a lack of oxygen with certain physiological changes, such as altered heart rate and movement.
Subscribe for FREE to the HealthTimes magazine
It is important to note, however, that factors other than lack of oxygen (e.g. maternal smoking, fetal anomalies and fetal sleep-wake cycles) can affect fetal physiological measurements.
Who gets fetal surveillance?
Fetal surveillance is recommended in pregnancies deemed at higher risk of fetal demise. This may include the following situations:
-
Twin pregnancy
-
Decreased fetal activity
-
Postterm pregnancy
-
Fetal growth restriction
-
Increased or decreased amniotic fluid volume
-
Preterm premature rupture of membranes
-
Past history of fetal demise
-
Certain medical conditions in the mother (e.g. diabetes, hypertension, pre-eclampsia, systemic lupus erythematosus, sickle cell disease, antiphospholipid syndrome, substance abuse, morbid obesity)
-
Rhesus D alloimmunisation
Which tests may be involved in fetal surveillance?
-
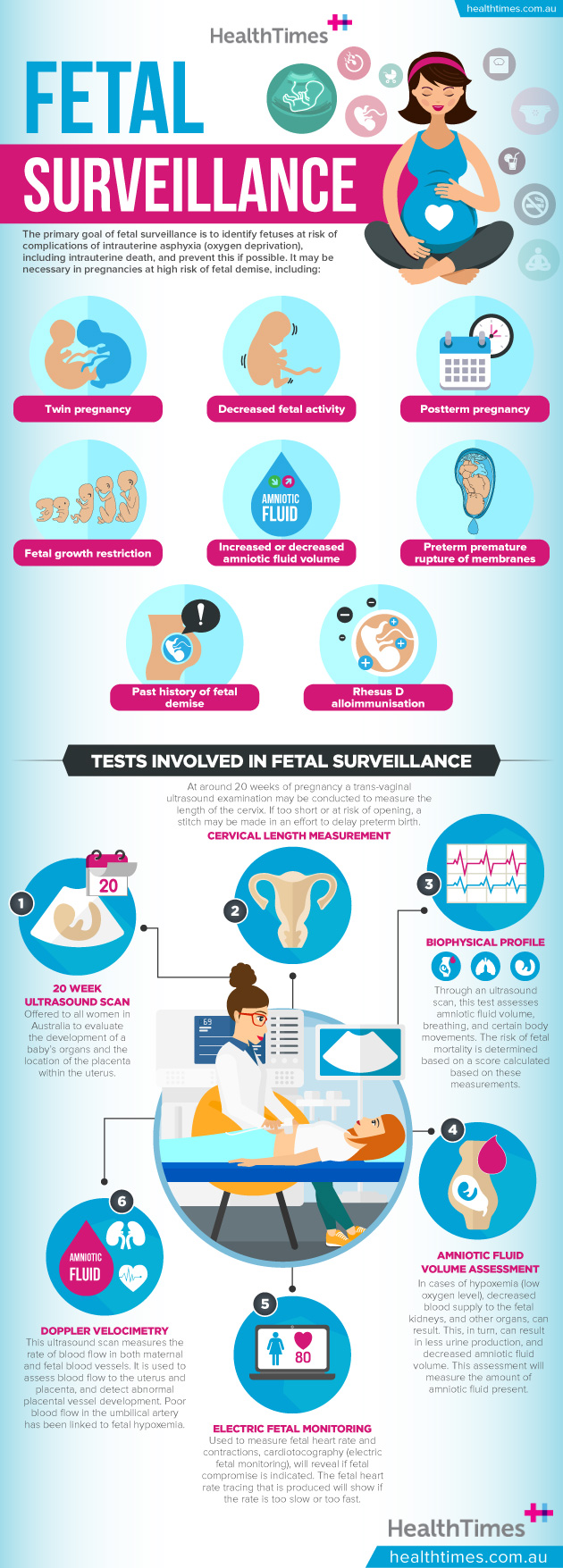
20-week anatomy ultrasound scan: A routine ultrasound scan, offered to all women in Australia to evaluate the development of the baby’s organs and the location of the placenta within the uterus. Cervical length may be measured at this time too (see below). Any abnormalities detected in this scan may prompt further fetal surveillance tests during the pregnancy.
-
Measurement of cervical length: Currently, at around 20 weeks of pregnancy, it is often routine to offer women a trans-vaginal ultrasound examination, in order to measure the length of the cervix. At this stage of pregnancy, cervical length is on average around 40mm (though this can vary widely), however a length of less than 25mm is linked with a greater risk of preterm birth. If the cervix is seen to be too short or at risk of opening, a cervical stitch may be put in to try to delay preterm birth.
-
Fetal movement count: A mother’s objective assessment of the movements of the fetus (decreased when the fetus experiences hypoxemia). It is recommended that women who notice a decrease in fetal movements should undergo further fetal surveillance. However, according to current evidence, there is no clear threshold for fetal movement that indicates when a fetus is at risk.
-
Biophysical profile/modified biophysical profile: This test involves fetal assessment through an ultrasound scan, which assess amniotic fluid volume, breathing movements of the fetus, and specific body movements (such as fetal tone, extension, flexion and reflex). Amniotic fluid volume is assessed and cardiotocography (for the modified biophysical profile) may also be required (these are both described below). A score is calculated based on these measurements and the risk of fetal mortality is based on this score.
-
Amniotic fluid volume assessment: In hypoxemia (low oxygen level), blood in the fetus is primarily directed towards the brain and heart and away from other organs such as the kidney (seen as less vital). Decreased blood supply to the fetal kidney results in less urine production, which in turn can result in decreased amniotic fluid volume (also known as oligohydramnios). The amount of amniotic fluid present can be measured in an ultrasound scan.
-
Cardiotocography/electronic fetal monitoring: This involves a belt with two plates (transducers) being placed on the mother’s abdomen. One plate measures fetal heart rate and the other measures abdominal pressure/contractions. A fetal heart rate tracing is produced. Fetal compromise is indicated when the fetal heart rate is either too slow or fast, or does not vary much in range. Normally, fetal heart rate varies between 110-160 beats/minute.
-
Doppler velocimetry: This test is a form of ultrasound scan that measures the velocity of blood flow in both maternal and fetal blood vessels. Blood flow to the uterus and placenta can be assessed and abnormal placental vessel development can be detected. For example, in cases of fetal growth restriction, reversed or absent diastolic blood flow in the umbilical artery is linked with fetal hypoxemia and increased fetal morbidity and mortality.
How long does fetal surveillance take?
Fetal surveillance tests should be performed on a regular basis until the time of delivery, if the condition that necessitated fetal surveillance is still present. The time between tests varies. It generally occurs weekly, but may occur more often if the fetus is seen to be at higher risk of complications.
What happens if the tests show an abnormality?
If the fetus is deemed to be at risk of morbidity or mortality, the baby’s delivery date may be brought forward if deemed beneficial by doctors. The other option is to continue monitoring the baby with regular fetal surveillance tests such as ultrasound scans or Doppler studies until the baby improves.




Comments